In our 27 years’ experience of supporting people following a spinal injury, one of the greatest concerns many of our spinal injury clients have is developing autonomic dysreflexia (AD). This sudden rise in the person’s blood pressure can have severe and even fatal consequences, and careful monitoring and prevention is vital, alongside rapid action should the person experience an episode of AD to ensure they have the best chance of recovery.
Does everyone with a spinal injury develop autonomic dysreflexia?
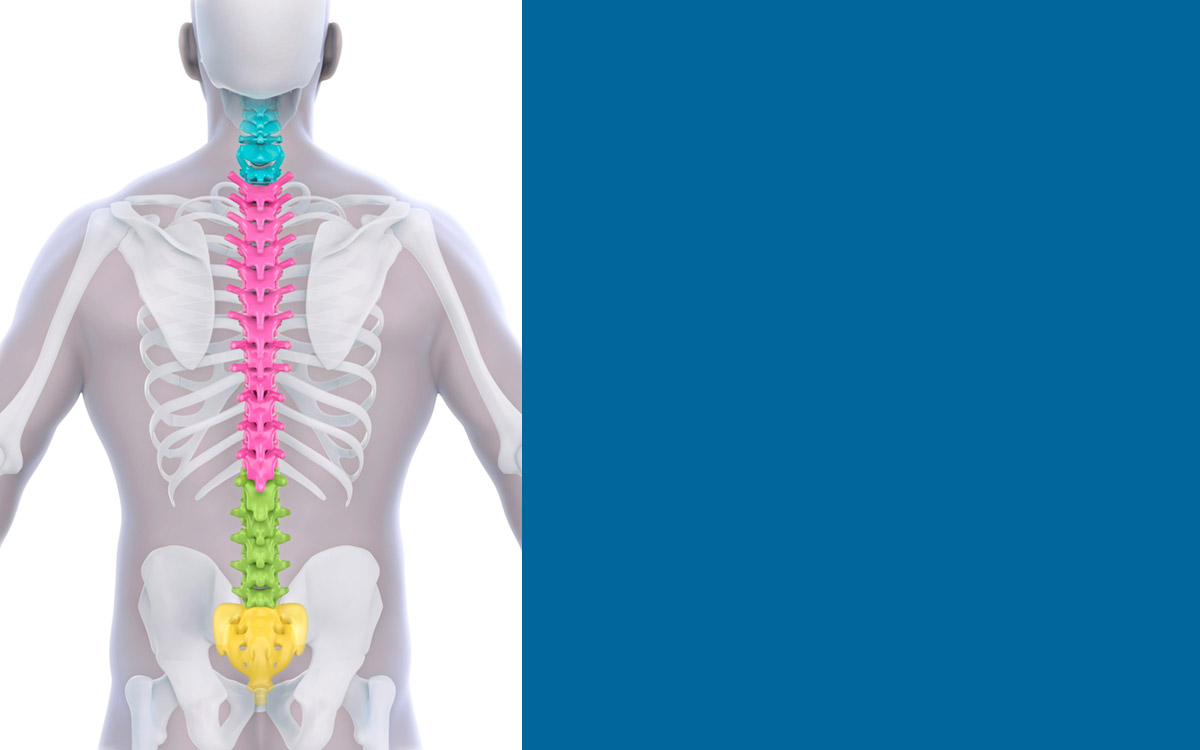
Autonomic dysreflexia is most common in people who have a spinal injury that is at T6 or above. It is caused when a noxious stimuli (an actual or potential tissue damaging event) occurs below the level of the person’s injury, so the higher the injury the greater the risk. It can be traced to circumstances that can be fairly innocuous in themselves, for example: wearing clothing that is too tight or digging into the person’s skin, the person needing to empty their bladder and/or bowel, the person engaging in sexual activity, or the person’s environment changing from very hot or very cold quickly (for example, going from a heavily air-conditioned inside area to a very hot outside area).
When a person with a spinal injury experiences a noxious stimuli, their body reacts in two different ways depending on the part(s) of the body affected by the stimuli. When a stimuli is detected in the areas of the body above the injury site, the blood vessels dilate to allow the blood pressure to return to a normal range, but below the injury site the messaging about the stimuli is halted, leaving the person’s blood pressure high until the noxious stimuli is removed.
Symptoms of autonomic dysreflexia
The person’s heart-rate slows and potentially becomes irregular, and alongside this the person may experience a pounding headache, cold and clammy skin below their spinal injury (perhaps accompanied by goose bumps), sweating above their spinal injury (perhaps accompanied by a flushed face), nausea and/or a blocked nose, impaired vision, and there may be signs of a pressure injury developing with red marks on the person’s skin.
All of our spinal injury live-in carers are highly trained to recognise these symptoms, and all of our spinal injury clients are regularly assessed to determine their autonomic dysreflexia risk-factors and identify any specific triggers.
How to treat autonomic dysreflexia
Every person we support who is at risk of autonomic dysreflexia has a rapid treatment plan that we follow in the event of them developing AD. Every plan is personal to the individual, but procedures that are often required include:
• Ensuring that the person is sat as upright as possible (with legs lowered).
• Tight clothing/shoes, jewellery and/or bandages etc are removed swiftly and the person’s skin checked for any signs of redness that might indicate the development of a pressure ulcer.
• Supporting the person to empty their bladder or bowel as per their individual care plan.
• Supporting the person to take any medication that is used in the event of an episode of autonomic dysreflexia, for example a GTN spray that helps to widen the person’s blood vessels.
• Continuous blood pressure monitoring to see if the person’s autonomic dysreflexia is alleviating or worsening after following the procedures to try and identify and treat what is causing their AD.
• Seeking further care urgently as necessary – this may mean calling 999.
Preventing autonomic dysreflexia
By identifying the person’s risk factors and triggers for autonomic dysreflexia during the formation of their personalised care plan, we aim to support the person to avoid episodes of AD as much as possible. Ways we do this include supporting the person to:
• Adhere to their personalised bladder and bowel management plan.
• Keep their skin healthy and avoid pressure ulcers.
• Support and advise the person to choose clothing that keeps them comfortable and isn’t tight or digging into them.
• Ensure that the fitting of any devices and/or bandages doesn’t constrict any part of their body.
If, despite this, the person does develop autonomic dysreflexia we know that swift treatment is absolutely vital to try and prevent a stroke, seizure or death. All of our live-in spinal injury carers are skilled at responding immediately to any signs or symptoms of autonomic dysreflexia, and supporting the person comprehensively to ensure the best outcome from an episode of AD.
Please visit the Spinal Injuries Association for additional information about autonomic dysreflexia.
Find out more about how ENA Care Group could support you or your family by calling 08004 334 413 or emailing care@ena.co.uk.